Insight Paper January 31, 2017
How Repeal of the Affordable Care Act May Impact Medicare Access and Chip Reauthorization Act
Touching on the “financial impact” to healthcare payers and providers and the implementation of MACRA.
Background
As the first act in his administration, President Trump signed an Executive Order that instructed federal agencies to take all action allowable by the law in order to waive, defer, grant exemptions from or delay the implementation of any provisions or requirement of the Affordable Care Act (ACA) that would impose a financial burden until legislation to repeal and replace the ACA is enacted. These changes will be implemented using the current notice and comment rulemaking process.
Note that the actions are for provisions with a “financial impact” and that the regular rulemaking process will be used to make these changes. It is unclear from the Order which particular provisions are impacted, but it is unlikely that the changes will impact the 2017 benefit year. In fact, most rates for 2018 are due to state departments of insurance this spring and the rules are unlikely to be changed before then. This Order is really intended to signal to the American people that changes are coming.
Given that political perspective, what decisions and actions should be taken by healthcare providers and health insurance plans now? Should they continue to move forward or stop and hope for a return to the days of fee-for-service medicine?
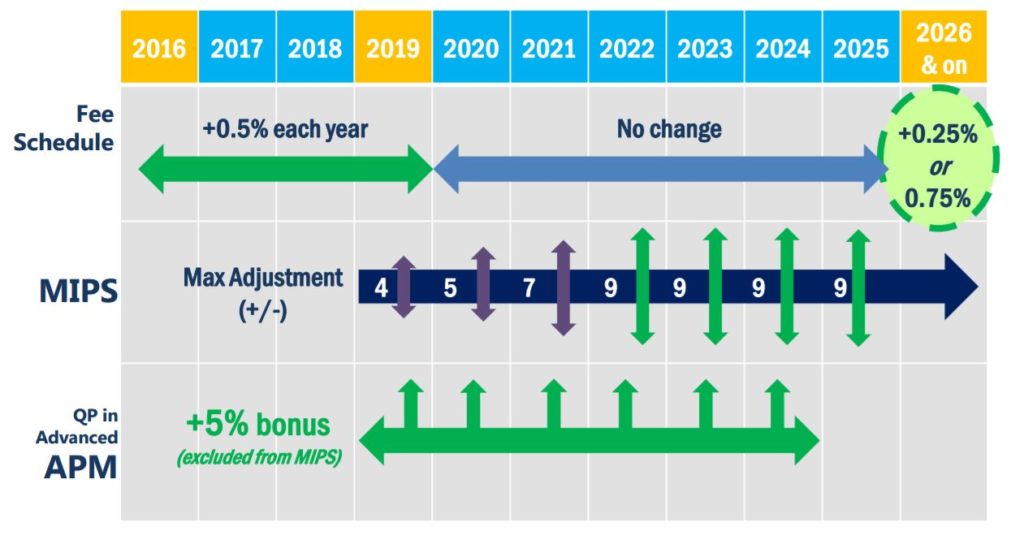
Even with its faults, ACA moved the healthcare industry to explore alternative reimbursement models designed to move away from traditional fee-for-service medicine – and that shift continues. Healthcare insurers continue to write more contracts with healthcare providers (hospitals, doctors, physician groups, etc.) which measure quality and reward positive outcomes through value-based care (VBC). These contracts reward hospitals and doctors for achieving the triple aim of improving quality, increasing patient satisfaction, and lowering costs. The Medicare Access and CHIP Reauthorization Act (MACRA) put a specific timeline on the rewards and penalties for VBC, with reporting data starting January 2017 with resulting rewards or penalties in 2019.
https://www.healthit.gov/FACAS/sites/faca/files/Quality-Payment-Program-MACRA-NPRM-Slides.pdf
How Does Repeal Affect MACRA
While the ACA has been a controversial law, MACRA was a bipartisan bill and has not received much attention in the press. MACRA was the solution to the Sustainable Growth Rate (SGR) which was a piece of legislation that Congress repeatedly “adjusted” each year to avoid drastic provider payment reductions. MACRA rests on the principle of the need for more value-based care, including measurement of quality and payments based on outcomes and not volume. Repeal of the ACA will present challenges to the implementation of MACRA.
While there are many parts of the ACA, the provisions that supported MACRA and the shift to value-based care are:
- The creation of the Centers for Medicare Medicaid Innovations (CMMI) – It allows for the implementation of new programs without passing legislation, therefore speeding up innovations.
- Medicare Shared Savings Programs (MSSP) – a program which creates incentives and penalties for physicians who come together to create Accountable Care Organizations (ACO) which are responsible for overall care and coordination of their patients. Some of these MSSPs allow the ACOs to qualify as Advanced Payment Models (APM) under MACRA.
- Creation of quality programs which are leveraged by MACRA’s to measure providers who are not involved in an eligible APM.
Over half of providers don’t understand that the MACRA law will be shifting their Medicare payments towards a more VBC approach. For these providers, potential delays in the implementation of MACRA will be welcome news. On the other hand, a number of providers have invested heavily in the creation of ACO’s in response to the ACA. While the ACO models created for the MSSP have had mixed results, the idea of a value-based model has bi-partisan appeal.
Much of the debate about what replaces the ACA has been focused on Health Savings Accounts (HSA), selling insurance across state lines and block grants for Medicaid. Value-based care appears to have taken a back seat.
In the coming weeks, we will learn more about the attitude of the new administration toward value-based care. If repeal of the ACA means the loss of CMMI this will likely undermine much of the infrastructure ACO’s and some providers have put in place to move toward a world of value-based care. Loss of this infrastructure would also challenge the ability of MACRA to achieve its savings goals. For now, it is likely that some payers and providers may hold back on additional investments in order to hedge their bets against an uncertain value-based future.

