Insight Paper November 4, 2021
Delineating Health Equity Programs
An assessment of the 25 largest US Healthcare Payers’ Health Equity Programs.
In a recent Trexin Insight Paper (TIP), Aaron Faugstad took a deep dive into the definition of Health Equity (“HE”), and what it means for the healthcare industry. This TIP builds on that research by assessing the top 25 US Healthcare Payers (by market share) and their work to diminish disparities and advance HE for their members. To measure the current state, we developed a HE Rubric built off a framework from the National Quality Forum, and measured the top 25 US Payers’ HE Programs based on criteria organized around collaboration and partnerships, culture of equity, structure for equity, access to care, and quality of care. To conduct this research, we spent roughly 30 minutes per Payer analyzing public sources online including Payers’ websites, LinkedIn pages, media sources, and community pages.
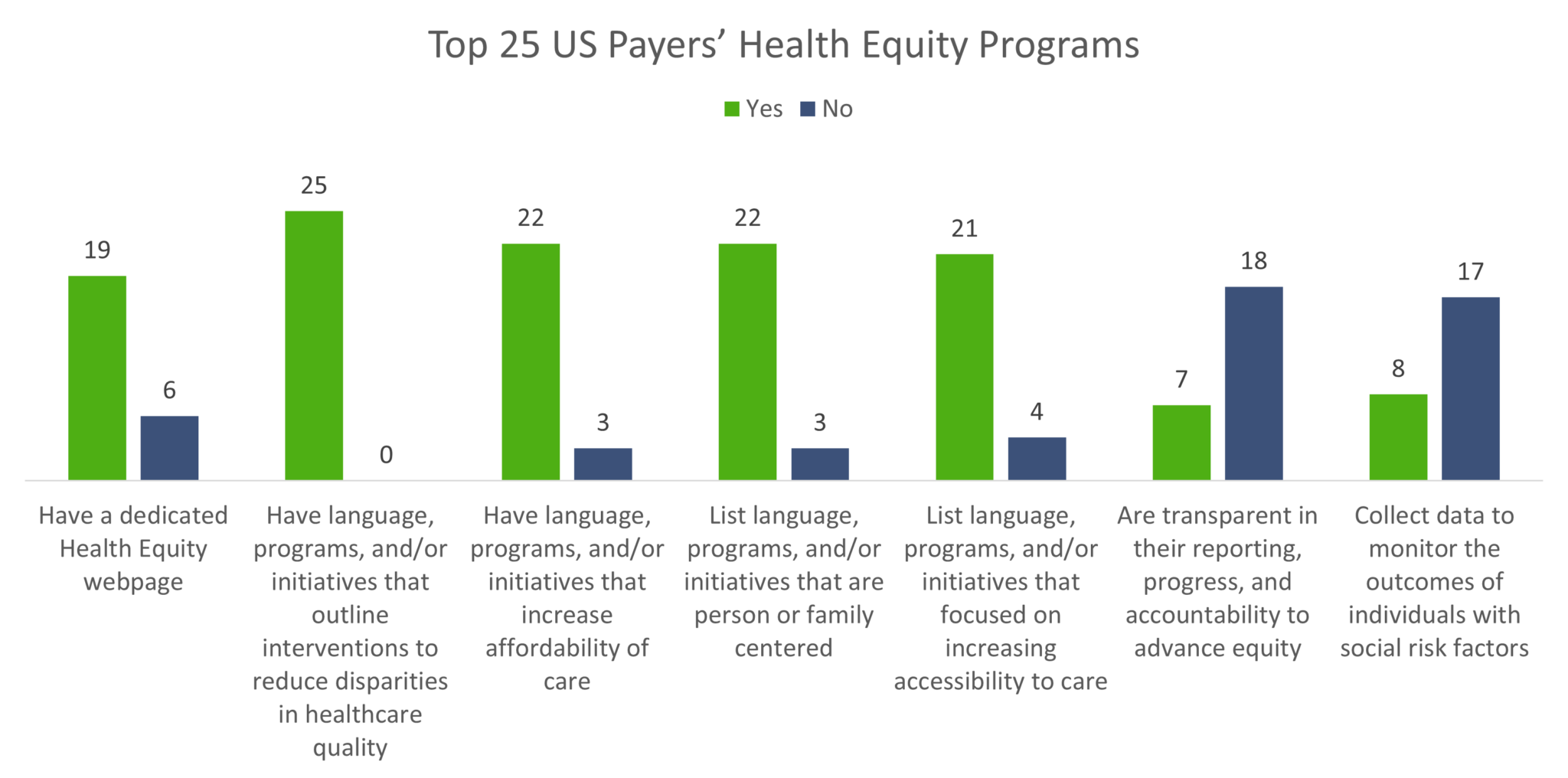
Here’s a highlight of what our research revealed:
Here is where our original framework was flawed:
25 out of the 25 Payers have language, programs, and/or initiatives that outline interventions to reduce disparities in healthcare quality
This seems obvious and should be expected from all Payers. Quality of care is a pillar of all Payer models. What our research and data failed to differentiate is if and how Payers are isolating HE data, initiatives, and governance to resolve quality of care disparities among members. Unspecific language resulted in a ‘Yes’ across the board in our Rubric. Upon auditing the data, results found that most Payers did have specific language describing Social Determinants of Health (SDoH), but from Payer to Payer were inconsistent in their use of language to describe HE data points or initiatives. Another finding builds upon this flaw:
19 out of the 25 Payers have a dedicated HE page
Or rather, six of the top Payers did not have a dedicated HE page. Because the framework originally applied only looked for language, programs, or initiatives that outline interventions to reduce disparities in healthcare quality, this question did not delineate language, programs, or initiatives that generally focus on quality of care from advancing quality of care focusing on a single health disparity area. This gap affected other areas of our research, including:
22 out of the 25 Payers had language, programs, and/or initiatives that increase affordability of care
22 out of the 25 Payers listed language, programs, and/or initiatives that are person or family centered
21 out of the 25 Payers listed language, programs, and/or initiatives that focused on increasing accessibility to care
While it is promising that the majority of the top Payers have language, programs, and/or initiatives around affordability of care, accessibility of care, and even person or family focused language, it suggests that the language, programs, and initiatives do not have a specific focus on advancing HE. The research revealed the difficulty in measuring HE programs, as quality of care and access to care are embedded within an organization. Again, our data revealed that Payers are thinking and acting on behalf of their members. Quality, affordable, and member-centered programming are base requirements for accreditation from the National Committee for Quality Assurance (NCQA), Utilization Review Accreditation Commission (URAC), and Healthcare Effectiveness Data and Information Set (HEDIS) measures. However, our interest is in HE specific programming. What our data revealed is our Rubric did not specifically call out the expected accreditation requirements of Payers. Accreditation standards are essential to ensure quality care is provided, but it is also the baseline expectation. Payers, and the framework that should support their HE initiatives and governance, need to consider how they can go above and beyond for their members.
What our data truly revealed:
To accurately measure and assess HE programs, a rubric must seek the specific data points and language that are essential to HE. Examples that we found from our research include:
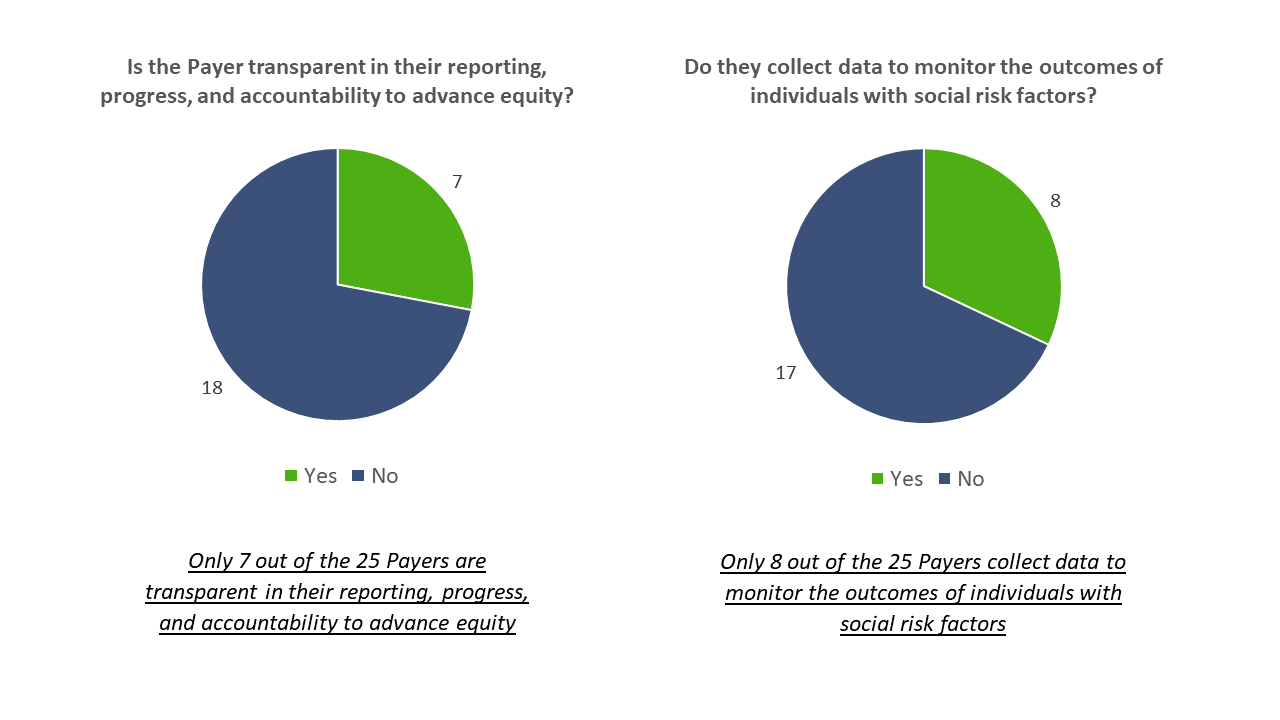
While there is the possibility that more Payers are collecting data to monitor the outcomes of individuals with social risk factors and are not transparent, these two examples demonstrate how to delineate HE related language and programs from broader initiatives within Payer organizations. In the current state, Payers have programs to improve access to care and quality of care. However, there are certain members that fall through the gaps of these existing programs due to social risk factors and SDoH. Therefore, the future state is organizing and executing initiatives to identify health disparities for members based on isolated HE data to address the gaps in the existing programs. The flaws in our research encouraged us to rethink our leading question: Should HE be embedded into existing data, initiatives, and governance, or should it be a separate entity through dedicated language, analytics, and frameworks?
The answer is both, technically.
The Trexin Way Forward
Due to the nature of collecting and isolating health disparity data, Payers will need to delineate and establish a HE Program. To do this effectively, a Payer must consider change management, program implementation, technology, data analytics, and project execution. Therefore, Payers must assess the current state of their HE programs by measuring the dedicated capabilities and resources which constitute the domains of a HE program. Although a HE program should have dedicated resources, eventually, Payers should integrate the HE program into their value-based care framework. To help Payers understand the current state of their own HE programs, we’ve shifted our Rubric to measure capabilities within the domains of HE to provide a more accurate assessment.
Trexin’s “EPIE” approach provides a full-scale HE program framework that can be used to assess, design, and implement a HE program, compartmentalized to apply to any Payer regardless of the current state. The “EPIE” methodology consists of the foundational work to Establish the HE program; Promote a culture of equity internally and collaborate with community partners to advocate externally; launch data team(s) to Identify health disparities and contextualize issue areas; and organize capabilities to Execute intervention projects to mitigate the identified areas of inequity. The end goal of Trexin’s EPIE is to integrate the HE program into an organization’s value-based care framework to ensure the program becomes a lasting, relevant, and valuable addition to an organization’s path to continuously improve quality of care. To learn more about our EPIE approach and updated HE program assessment, please click HERE.
If you would like more information on our methodology, our updated HE program assessment, or have other questions regarding this TIP, Isabelle and Aaron welcome any discussion. This is the second TIP in a series of three providing new insights into HE. Be on the lookout for the third TIP in early December!

