Case Study July 2, 2014
Data Science for a Safety Net Hospital
Understanding Mis-triage in Severe Sepsis Patients with Community Acquired infections
Business Driver
Community-acquired infections (CAI) are among the most common reasons for admission at regional safety net hospitals. CAI is emblematic of the types of choices that hospitals must make every day, there is variation in: patient risk factors; severity of symptoms on presentation; and the ultimate severity of the course of managed illness. When the emergency department is presented with a CAI case the first important triage decision is whether to manage the infection on an outpatient basis or admit the patient to the hospital. If the patient is admitted, the next choice is between care on the floor or admission to the intensive care unit (ICU). Patients requiring a higher level of care (such as mechanical ventilation) or who are seen as being at greater risk of rapid deterioration are admitted to the ICU with its more intense and often more expensive care. However, too often patients that start on the floor deteriorate in the next day or two and are moved to the ICU. Does this represent good resource allocation or mis-triage in assigning a patient to the wrong level of care, contributing to worse outcome. The regional safety net hospital in this case, wanted to answer these and other questions about the management of patients with severe CAI but didn’t have several years or millions of dollars budget to conduct it prospectively.
Approach
Since it was not possible to design and execute a prospective study, we chose to use data science to build a rapid prototype analysis using discharge abstracts and daily itemized billing data from the purchasing cooperative to which the hospital belonged. Working closely with business leaders, subject matter experts, and IT, the team defined the detailed study design and executed the analysis. Getting agreement on definitions, the conditions being evaluated and the metrics was important to the success of the effort. While detailed information on the physiology was not available from the resource use data, the actions taken by care providers in response changes were well documented: use of antibiotics by class and dose; location of care (entry through the ER and daily floor or ICU location); organ support (mechanical ventilation, vasopressor use, renal dialysis). Combined with discharge diagnosis information we could identify CAI and its most severe manifestation severe sepsis, infection with acute organ failures. The presence of relevant items was identified in the raw itemized data. Summaries were then created for each day of the hospitalization. Finally, a view was constructed from the days characterizing the chosen events. CAI was defined by ER use and antibiotic therapy on the first day of the hospitalization for cases where infection was documented in the discharge abstract. Mis-triage was defined as ICU- admission on the second or third day after initial floor care. Patients were characterized by their care patterns and a variety of metrics were summarized. Additionally, data from the institutions was used in order to increase the trust of the providers in the results.
Results
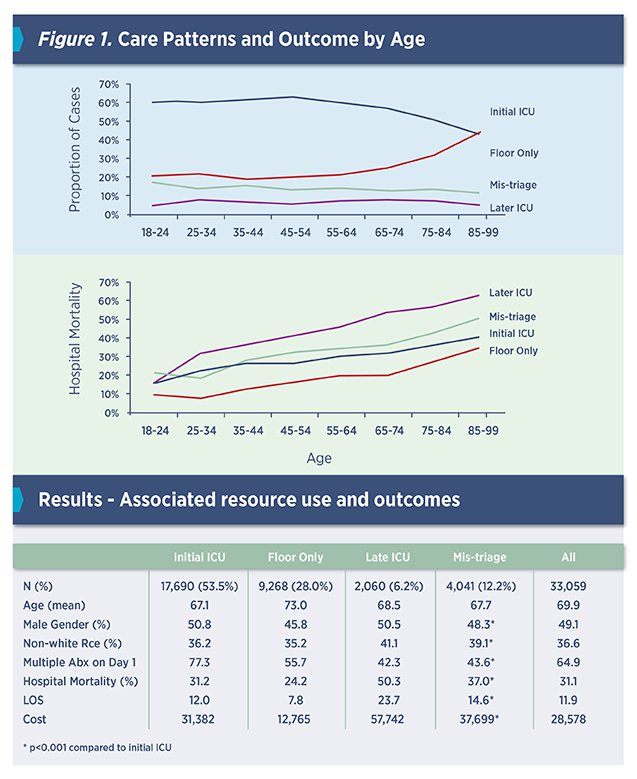
The analysis showed that mis-triage was common (1 in 8 patients). Mis-triage caused significantly greater resource use and increased mortality. We found mis-triage was more common in older patients, those without complex co-morbidity and those started on single rather than multiple antibiotic therapy. Surprisingly, we also found that smaller hospitals, had lower mis-triage rates. This was shared with the network and the hospitals that had better triage, their best practices could be applied to those hospitals in the network with greater rates of mis-triage. Finally, having identified specific cases at each hospital where mis-triage was observed in the administrative data, these cases were flagged for clinical review to see what might have lead to the decision to manage on the floor and whether multiple initial antibiotic therapy or other aspect of initial care might have avoided the ICU admission.