Insight Paper March 11, 2021
Could Drug Diversion Be Affecting You?
COVID-19 has put hospital systems at a higher risk.
The chances that you have encountered a healthcare professional in their workplace abusing or misusing narcotics at some point in their life is very high. It is estimated that one in ten nurses have this problem for a few reasons. To begin, healthcare professionals have one of the most stressful jobs. Nurses and doctors work long shifts and are trained professionals when it comes to drug knowledge. These professionals feel like they can use the drugs without becoming addicted and also see the positive effects they have on patients when administered to them.
Drug diversion impacts more than just the diverter involved; it effects patients, workplace safety, friends, and families. If a patient is in the presence of a drug diverter, it is obvious that they are getting suboptimal care, but they are also receiving insufficient pain control, and are at superior risk of infection. In one of the largest drug diversion scandals to date, a surgical technician from Rose Medical Center in Denver infected at least 18 patients with hepatitis C by stealing drugs from syringes and filling up the syringe with saline before administering to her patients. The technician was sentenced to 30 years in prison. The health and safety of patients are the most concerning outcome, but hospitals are also at high risk for costs, fines, and a reputation that could shut down the healthcare system.
With the research and technology available today, we are in a much better place to get drug diversion under control.
There are four main steps in assessing drug diversion at hospitals:
- The first step is to engage a drug diversion task force. This must be a multidisciplinary collaborative team that meets regularly to review suspicious activity, data, and works to improve processes and procedures throughout the organization. It is critical that this task force is comprised of individuals from the following teams: pharmacy, human resources, nursing, security, anesthesia, compliance, and legal.
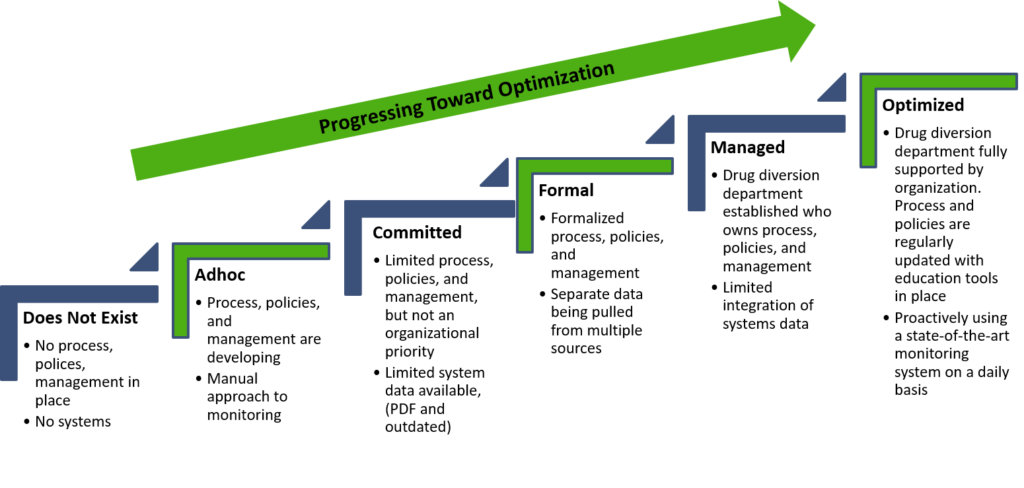
- The second step is to evaluate where the organization is and determine where you want to go. It is imperative that your senior leadership team is on the same page and is motivated to make drug diversion mitigation a top priority. Perform a gap analysis to see the main areas where your organization requires additional resources, processes, or technology to get to your future goal state.
- The third step in this process is to strategize ways to improve your drug diversion monitoring program. Once you have your strategy, your drug diversion task force team also begins to plan a roadmap to optimization success. For example, determining which third party software that has artificial intelligence learning capabilities would be best for your organization, establishing key performance indicators with all areas of the hospital and continually reassess and review, and have annual staff education trainings about signs and symptoms and how to report suspicious activities are all great strategies of how to best monitor drug diversion in your hospital.
- The final step in the process is to execute your plan and strategy. It is vital to have direct communication from the task force leadership and regular check ins with the organization to keep all healthcare professionals up to date on how the execution is tracking.
The maturity matrix below is a great starting point to assess how developed your organization is and steps you need to take in order to optimize your program.
In hospitals today, many pharmacy teams rely on manual audits for drug diversion detection. This is a problem for many reasons. First, it takes an unwarranted number of staff to filter through all kinds of different reports such as electronic health records for patient diagnoses and history, human resource information to see what types of access doctors and nurses have, automated dispensing cabinet to determine if controlled substances (CS) were administered, wasted, or returned, and surveillance tools. The challenge in this process is that it takes many hours to detect suspicious activity and by that time, you are most likely weeks or months down the road from the time the potential diversion happened. This process also leads to high false-positive rates which defeats investigators and makes it troubling for organizations to evaluate and improve their processes and procedures.
Ultimately, drug diversion prevention and management are about executive buy-in, realizing how much of an impact misuse and abuse of controlled substances can have on innocent patients, healthcare professionals, and the hospital itself. Executive leadership must educate and communicate how important it is to have processes and procedures in place and that they are followed. With clear goals, strategies, and implementation, the culture of drug diversion will be apparent and executed to ensure a healthy and safe healthcare system.

