Case Study December 14, 2017
Closing a $160M Financial Premium Subsidy Gap
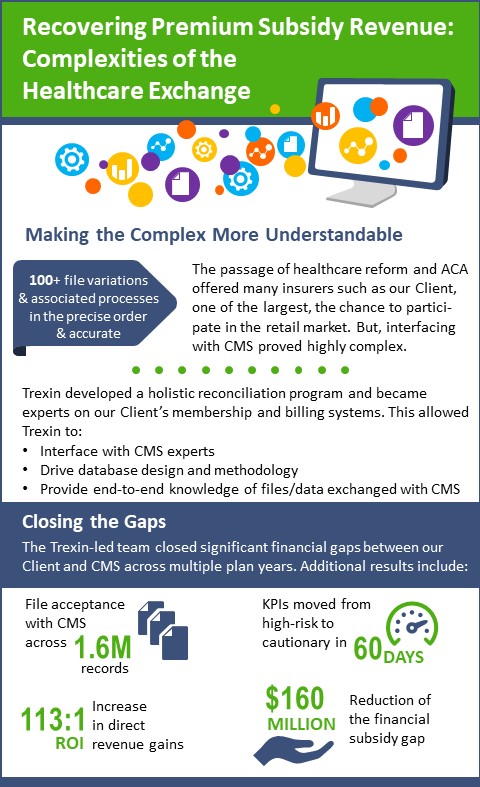
Trexin helped a large Healthcare Payer participating in public retail exchanges reduce its financial exposure and mitigate its audit risk.
Business Driver
When the federal government regulated healthcare reform through passage of the Patient Protection and Affordable Care Act (ACA), individual consumers not covered by health insurance were mandated to purchase healthcare insurance via the federal exchange or state-based exchanges. Health insurance issuers were encouraged to participate in this retail market by offering plans in these exchanges, but with it came immense complexities in operational management, data reconciliation and financial alignment across large membership bases. Our Client, one of the largest insurers, faced significant financial exposure and mounting audit risk from this retail healthcare exchange business because data was disparate among internal source systems, file processing was inconsistent and reconciliation with government agencies was strained. Given these challenges, the SVP of Operations engaged Trexin to lead a comprehensive reconciliation program to recover premium subsidy revenue across a base of nearly 1 million members and reconcile federal eligibility with the Centers for Medicare and Medicaid Services (CMS).
Approach
Trexin’s analysis revealed that our Client had been plagued by data discrepancy and reconciliation alignment with the federal government since entering the retail marketplace. This was understandable given that the interface with CMS is highly complex with over 100 file variations and associated processes that must be followed in precise order to accurately and efficiently communicate with the government to ultimately receive the appropriate subsidy reimbursement payments for each of the members an insurer serves in this line of business. Trexin’s approach was to develop a holistic reconciliation program incorporating cross-functional Client resources, Trexin subject matter experts specializing in the public healthcare exchange and best-in-class tools providing transparency for agile business decisions. Trexin quickly became the foremost internal expert of our Client’s membership and billing systems, drove underlying database design and methodologies, interfaced with CMS experts and provided end-to-end knowledge of all inbound and outbound files and data exchanged with CMS. With that foundation established, Trexin then drove closure of significant financial gaps between our Client and CMS across multiple plan years through targeted data dispute submissions and refinement of existing daily, weekly and monthly reconciliation files.
Results
The Trexin-led team achieved statistical validation and member eligibility file acceptance with CMS across 1.6M records, moving key business indicators from high-risk to cautionary within 60 days and driving eligibility dispute acceptance rates to 97%. Trexin ultimately reduced our Client’s financial premium subsidy gap by $160M, contributing to an increase in direct revenue gains and reduced financial reserves being held. For every $1 that was invested by our Client for our services, Trexin returned $113 to the bottom line.

