NCQA Stratifying HEDIS Measures by Race and Ethnicity
Preparing healthcare plans to comply with stratification of NCQA HEDIS measures by race/ethnicity for member year 2022.

WHAT HAS HAPPENED?
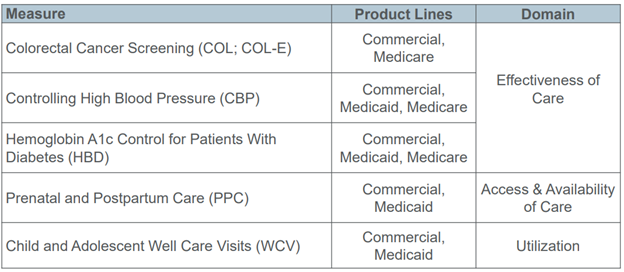
The National Committee for Quality Assurance (NCQA) has introduced its intent to require the stratification of five of its Healthcare Effectiveness Data and Information Set (HEDIS) measures – the United States’ most widely used healthcare performance tool – for member year 2022. The following measurements have been selected to categorize and organize Medicare, Medicaid, and Commercial members of an organization’s health plan(s) by their race and ethnicity.
WHO IS AFFECTED AND WHY?
As more than one-hundred ninety million members are currently enrolled in healthcare plans that provide HEDIS data – this change in standard portends to be both a significant opportunity and risk for healthcare providers in the United States. Providers across the nation have reason to pay notice to this adjustment as HEDIS is currently utilized by NCQA – the most recognized healthcare accreditation program in the United States, to measure care and service performance by healthcare plans as well as provide NCQA Health Plan Accreditation. NCQA Health Plan Accreditation is crucial for health plans to obtain to align with legal state requirements. Forty-two states use or require NCQA Health Plan Accreditation – and more than 75% of all insured Americans are enrolled in NCQA accredited plans.
WHERE IS THIS HEADED?
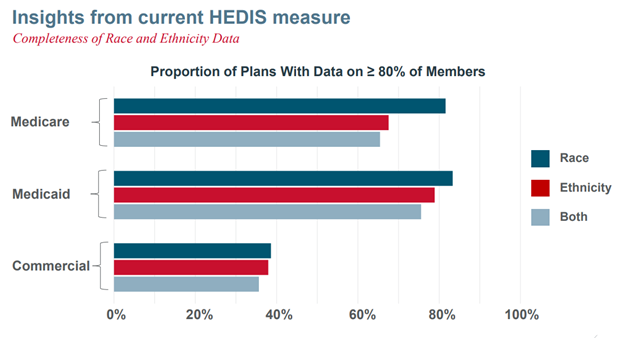
The NCQA has pledged to build equity into all of its programs and investigate inequitable care on a nation-wide scale – and expects to incorporate five more measurements in the following member years of 2023 and 2024. Beyond this, the NCQA expects that by member year 2024 healthcare plans will have 80% of their member population’s race and ethnicity data collected in order to comply with NCQA Health Plan Accreditation.
The NCQA has published data identifying that a significant number of healthcare plans are not prepared to meet these standards. Commercial plans seem especially at risk of not meeting NCQA’s upcoming standards and losing accreditation.
You can look forward to future Trexin Insight Papers (TIPs) detailing the exact steps Trexin is excited to take to help health plans commit to meeting NCQA standards and establishing Health Equity initiatives.
Trexin Advisors are prepared to help you understand and assess the status of your organization’s health plans’ NCQA accreditation, develop a roadmap, and execute an implementation plan to earn your accreditation if needed. Contact a Trexin Advisor and learn more today.
Source: https://www.ncqa.org/wp-content/uploads/2021/06/2021-0622-Future-of-HEDIS.pdf