Quantifying ICU Cost and Outcomes for the Uninsured
Trexin helped a large research hospital understand how the lack of insurance affects the usage of hospital resources, cost, and outcome of care by combining psychosocial and clinical data and examining the results

Business Driver
The lack of health insurance is often associated with reduced access to many health services. However, the relationship between lack of insurance and use of intensive care unit (ICU) services is unclear. Our Client, a large research hospital, believed that the absence of health insurance had the potential to delay treatment, resulting in a higher cost for care and outcomes that were worse than those who had insurance. Because one in six Americans over 65 does not have health insurance, our Client felt that a better understanding of the impact would allow them to present lawmakers with better information leading to better laws surrounding healthcare and healthcare reform.
Our Client asked Trexin to help them to find a way to better understand how hospital and ICU resources are used when accounting for age, gender, ethnicity, income, and insurance status and determine the effects that the lack of insurance has on cost and outcome.
Approach
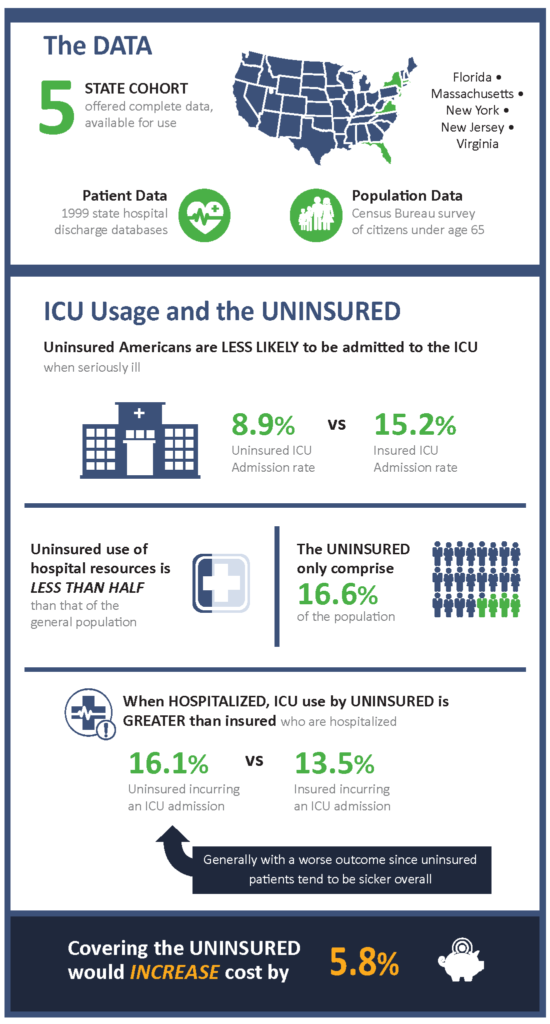
Because the design of the study was to be a retrospective, population-based, and cross-sectional examination of Americans under the age of 65, we needed to have access to data about the population in a specific region, which we could gather from the Census Bureau Current Population Survey. But we also needed the hospital discharge information for that same region to get the entire picture. Fortunately, we found that the 1999 state hospital discharge databases from Florida, Massachusetts, New Jersey, New York, and Virginia were not only complete enough for us to conduct our analysis, but also available for us to use in our study.
From the five state hospital discharge databases, we were able to collect important clinical data, including cost-to-charge ratios and detailed hospital characteristics from the Medicare cost reports. We were also able to gather essential patient information. Age, gender, ethnicity, payer, ICU room charges, discharge diagnosis, and hospital discharge status were all available to us. The census information gave us the current population survey data of people under the age of 65 from the five states and contained age, gender, and ethnicity-specific estimates of the number of the total population and the number of uninsured for the five study states.
When we brought together the hospitalization data and the population data, we were able to calculate the age, gender, and ethnicity-specific hospital and ICU admission rates and hospital mortality for our five-state cohort and examine the impact that the lack of health insurance had on cost and outcome of care.
Results
Overall, uninsured Americans are less likely to be admitted to the hospital when seriously ill, and their use of hospital resources is less than half than the general population. Use of ICU services by uninsured patients is also significantly lower than insured patients overall. But when admitted to the hospital, ICU use by the uninsured is greater than insured patients who are hospitalized, and the outcome is worse, possibly because they are sicker when they seek care. Based on the types of care received and the worse outcomes, the uninsured patients that are admitted to the hospital are sicker overall. We determined that covering the uninsured would increase the cost of ICU care by 5.8% despite the fact that the uninsured make up only 16.6% of the population.
With this information, our Client was able to provide useful data to lawmakers so that they could make informed decisions on new healthcare-related legislation.